ABSTRACT
This case report describes a 73-year-old Caucasian man who had COVID-19 and developed chronic, severe pruritus. The patient’s pruritus did not respond to numerous conventional and unconventional treatments, highlighting the difficulty of treating post-COVID-19 dermatological symptoms. Pruritus in the patient was significantly reduced with dupilumab, a monoclonal antibody that inhibits interleukin-4 and interleukin-13 signaling. The report describes the history of the patient’s pruritus, from the development of symptoms after COVID-19 infection through several treatment modalities that were not effective, and, finally, the resolution of the patient’s symptoms after starting dupilumab. The patient’s recent SARS-CoV-2 infection may have caused the immune-mediated process shown by the patient’s histopathological results. Even though these results are based on a single case, they highlight COVID-19’s ability to cause chronic pruritus and dupilumab as a possible treatment approach. Further study is needed to confirm these findings and investigate possible immunological connections between COVID-19 and chronic pruritus.
Keywords: COVID-19, pruritus, geriatric dermatology
INTRODUCTION
Pruritus, also known as itchy skin, is an uncomfortable sensation that prompts scratching.1 It can develop in several clinical situations, such as dry skin, skin conditions like eczema and psoriasis, systemic diseases, medication side effects, psychological factors, and unknown causes.1 Chronic pruritus is itching that persists beyond six weeks.2 Pruritis has been linked to several COVID-19-related skin conditions,3 with the most common rashes being morbilliform rash, urticaria, pseudo-chilblains, and vaso-occlusive lesions.4 This case report emphasizes the onset of pruritus four weeks post-COVID-19 infection; its significance lies in the patient’s severe and persistent condition and the numerous unsuccessful treatments.
CASE
A 73-year-old Caucasian man developed significant pruritus across his body, starting four weeks post-COVID infection. SARS-CoV-2 antibody IgG was positive four weeks prior to the onset of the rash. Urticaria preceded the presentation of cutaneous findings of multiple brown and pink macules and papules (3–6 mm) on his trunk and erythematous papules and patches on his arms, legs, and trunk; the rest of his skin examination was within normal limits (Figure 1). No travel history, dietary changes, or new skincare products were reported.

Figure 1. Erythematous papules and patches on the right lower leg.
Two 4-mm punch biopsies were taken from his legs. Biopsies showed spongiotic dermatitis with lymphocytic inflammatory infiltrate, lacking other significant inflammatory cells, with red blood extravasation (Figure 2). The patient was advised to switch to hypoallergenic detergent and skin care, avoid hot showers, and start oral hydroxyzine and topical triamcinolone.
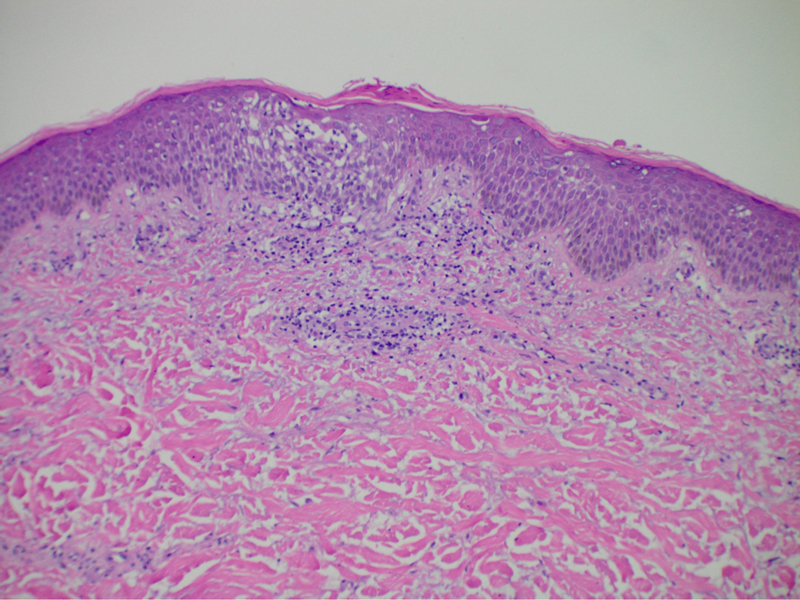
Figure 2. Spongiotic dermatitis with modrate lymphocytic infiltrate.
He noted minimal improvement with triamcinolone. The patient reported that triamcinolone 0.1% cream reduced his pruritus score from 6 to 3 out of 10. Pruritus was worse at night, mainly affecting the trunk and extremities. His primary care practitioner prescribed fexofenadine, cetirizine, montelukast, and cimetidine daily, but without relief. Five months later, a naltrexone trial began, and laboratory tests were ordered to exclude autoimmune conditions. Erythrocyte sedimentation rate and C-reactive protein levels were within normal range, and the anti-nuclear antibody test was negative.
After a trial of naltrexone proved ineffective, a two-week trial of doxycycline was attempted due to the patient’s hot tub use and rash severity on his thighs. Despite being the preferred treatment for bacterial folliculitis, it failed to alleviate his pruritus. After six months of unsuccessful treatments, the patient started twice-weekly phototherapy, with no improvement after three months. A trial with dupilumab was considered due to the debilitating rash. Six weeks post-dupilumab initiation, the patient reported a 50% pruritus reduction and had only one flare. The provider informed the patient that dupilumab typically takes 10–12 weeks to work, so early improvement was promising. After six months of treatment with dupilumab, the patient’s symptoms entirely resolved.
DISCUSSION
This case report details the difficulties in treating pruritus in a COVID-19 patient. This elderly patient developed prolonged pruritus four weeks post-infection, which persisted despite treatment. He was advised to avoid hot showers and allergenic skin care products. Oral hydroxyzine and topical triamcinolone were unsuccessful. Biopsy revealed spongiotic dermatitis with lymphocytic inflammation, possibly contributing to persistent pruritus. Fexofenadine, cetirizine, montelukast, cimetidine, naltrexone, and doxycycline did not improve his symptoms. Bi-weekly phototherapy was ineffective. After multiple treatment failures, dupilumab was prescribed and resolved his symptoms in ten weeks. This case suggests dupilumab could be a potential solution for COVID-19-related pruritus, which can cause severe, prolonged pruritus post-viral infection, persisting despite various treatments.5
Recent research indicates that COVID-19-related pruritus is not histamine-mediated, and this potentially explains why first-line treatments for pruritus failed to alleviate symptoms.6 COVID-19 pruritus is linked to epidermal interleukin 31 (IL-31) expression, a cytokine responsible for modulating immunological responses associated with chronic pruritus.6 Dupilumab, a monoclonal antibody, inhibits interleukin-4 (IL-4) and interleukin-13 (IL-13) signaling and is commonly used to treat atopic dermatitis by reducing IL-13 levels in atopic patients.7,8 Another study found that dupilumab completely blocked IL-4R expression and signaling associated with IL-31 production.9 Although these trials suggest a link between dupilumab and IL-31, more study is needed. The histology of this rash resembled eczema, often associated with severe itching.10 Histological examination revealed a moderate primarily lymphocytic infiltration with spongiosis of the epidermis without evidence of vasculitis (Figure 2), a histological pattern common in chronic pruritis.6 This likely caused the patient’s persistent, 10-month-long rash. The final diagnosis for this case is chronic pruritis secondary to viral infection.
CONCLUSIONS
This case documents a connection between COVID-19 and chronic, severe pruritus resistant to multiple treatments. Histopathology suggested an immune-mediated process, potentially tied to recent COVID-19 infection. The patient’s response to dupilumab, which inhibits interleukin-4 and interleukin-13 signaling, suggests an immunological basis for this pruritus. This case emphasizes the need for further research and effective treatment strategies and demonstrates the complications and challenges in managing complex dermatological post-COVID symptoms. However, this report involves a single case, and further study is needed on the connection between COVID-19 infections and chronic pruritus.
ACKNOWLEDGMENTS
We want to thank all involved in this case for their support and willingness to participate in this patient’s care. We also want to thank the patient for allowing us to use his case and findings to inform clinicians.
REFERENCES
- Song J, Xian D, Yang L, et al. Pruritus: progress toward pathogenesis and treatment. Biomed Res Int 2018;2018:9625936.
- Pogatzki-Zahn E, Marziniak M, Schneider G, et al. Chronic pruritus: targets, mechanisms and future therapies. Drug News Perspect 2008;21(10):541–551.
- Galván Casas C, Català A, Carretero Hernández G, et al. Classification of the cutaneous manifestations of COVID-19: a rapid prospective nationwide consensus study in Spain with 375 cases. Br J Dermatol 2020;183:71.
- Polly S, Fernandez AP. Common skin signs of COVID-19 in adults: An update. Cleve Clin J Med 2022;89:161–7.
- Weisshaar E, Szepietowski JC, Darsow U, et al. European guideline on chronic pruritus. Acta Derm Venereol 2012;92:563–81.
- Labib A, Nattkemper LA, Vander Does A, et al. COVID-19-associated pruritus is non-histaminergic mediated. J Invest Dermatol 2022;142:B38.
- D’Ippolito D, Pisano M. Dupilumab (Dupixent): An interleukin-4 receptor antagonist for atopic dermatitis. P T 2018;43:532–5.
- Kishi R, Toyama S, Tominaga M, et al. Effects of dupilumab on itch-related events in atopic dermatitis: implications for assessing treatment efficacy in clinical practice. Cells 2023;12:239.
- Bakker DS, van der Wal MM, Heeb LEM, et al. Early and long-term effects of dupilumab treatment on circulating t-cell functions in patients with moderate-to-severe atopic dermatitis. J Invest Dermatol 2021;141:1943–53.
- Houck G, Saeed S, Stevens GL, Morgan MB. Eczema and the spongiotic dermatoses: A histologic and pathogenic update. Semin Cutan Med Surg 2004;23:39–45.
Article citation: Meltan S, Matthew E, Tarbox M. Revealing the therapeutic potential of dupilumab: a case report on managing post-COVID-19 chronic pruritus in a geriatric patient The Southwest Respiratory and Critical Care Chronicles 2023;11(49):27–30
From: School of Medicine (SM), Department of Dermatology (EM, MT), Texas Tech University Health Sciences Center, Lubbock, Texas
Submitted: 8/14/2023
Accepted: 10/7/2023
Conflicts of interest: none
This work is licensed under a Creative Commons
Attribution-ShareAlike 4.0 International License.