Abstract
Acute decompensated heart failure in the setting of cavotricuspid isthmus-dependent atrial flutter and thyroid storm
Cristian Castillo MD, John Abdelmalek MD, Michel Juarez MD
Corresponding author: Cristian Castillo
Contact Information: Cristian.Castillo-Rodriguez@ttuhsc.edu
DOI: 10.12746/swrccc.v12i51.1315
ABSTRACT
Thyroid storm is an extreme form of hyperthyroidism associated with a high mortality rate. Heart failure is considered the leading cause of mortality in these patients. Atrial flutter is the second most common arrhythmia in patients with thyroid storms that can lead to cardiomyopathy and further complications, such as acute decompensated heart failure. In this report, we present a case of acute decompensated heart failure in the setting of cavotricuspid isthmus-dependent atrial flutter and thyroid storm.
Keywords: Thyroid storm, Graves’ disease, cardiomyopathy, atrial flutter
BACKGROUND
Thyroid storm, a rare but life-threatening complication of hyperthyroidism, can profoundly affect the cardiovascular system. Potential complications include atrial arrythmias and cardiomyopathy. An overactive thyroid gland releases excessive thyroid hormones into the bloodstream, stimulating myocytes and triggering atrial flutter and cardiomyopathy, which are conditions that damage heart muscle and ultimately can lead to cardiogenic shock.
CASE
A 31-year-old man with a history of Graves’ disease presented to the emergency department with a history of two months of palpitations, fever, shortness of breath, bilateral lower extremity edema, neck swelling, irritability, and unintentional weight loss of 180 pounds in the prior 18 months. The physical examination showed fever (103°F), tachycardia (160 bpm) (Figure 1), bilateral lid lag, fine tremors of the outstretched hands, global brisk reflexes, hyperdynamic precordium, and lower lung field crackles. Workup showed TSH < 0.01 microunits/mL (range: 0.27–4.20), free T4 > 7.7 ng/dl (range: 0.93–1.70), free T3 21.7 pg/mL (range: 2.3–4.1), troponin-T 10.9 ng/L (range: 0–19.0), BNP 8,178 pg/mL (<124). A transthoracic echocardiogram showed reduced left ventricular ejection fraction (LVEF) of 35% with no regional wall motion abnormalities and electrocardiogram with atrial flutter (Figure 2). The patient was transferred to the intensive care unit due to thyroid storm with a Burch-Wartofsky score of 85 and cardiogenic pulmonary edema secondary new onset heart failure with a reduced ejection fraction. The patient received high-dose hydrocortisone, methimazole, esmolol infusion, and due to persistent cavotricuspid isthmus-dependent atrial flutter was successfully treated with ablation (Figure 3).
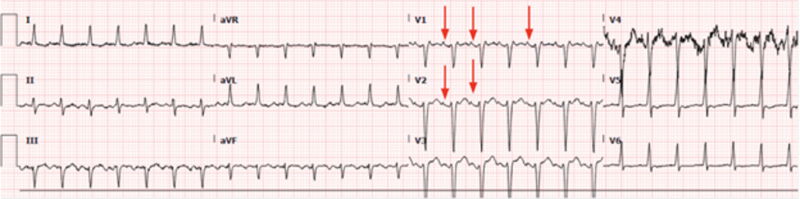
Figure 1. Admission ECG: Sinus tachycardia.
In leads V1 and V2 there are clear normal P waves regularly followed by a narrow QRS with a frequency of 166 bpm.
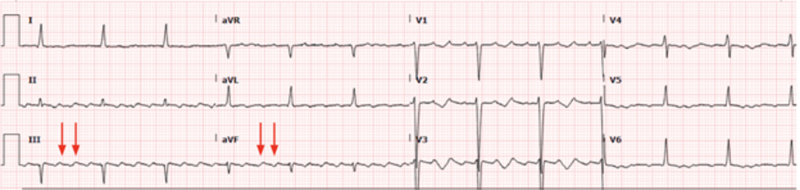
Figure 2. Pre-ablation ECG: atrial flutter 3:1 conduction.
In leads III and aVF, evidence of shark waves characteristic of atrial flutter with 3:1 atrioventricular conduction rate.
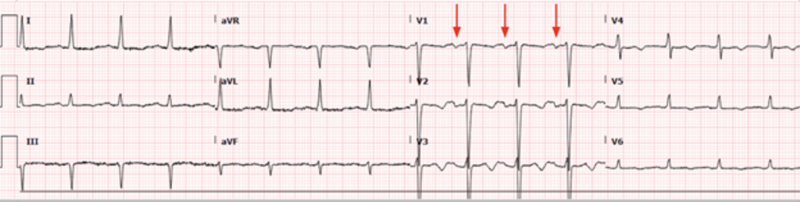
Figure 3. Post ablation ECG: sinus rhythm.
In lead V1 there are clear normal P waves regularly followed by a narrow QRS with a frequency of 93 bpm.
INVESTIGATIONS
During his ICU admission, continuous telemetry showed atrial flutter confirmed with a 12-lead ECG (Figure 2). Based on the CHF exacerbation of possible tachycardia-induced cardiomyopathy, electrophysiology consultation service decided to pursue an atrial flutter ablation.
DISCUSSION
Thyroid hormones (TH) have a complex relationship with the cardiovascular system through multiple mechanisms, including effects on myocardial mechanics (heat rate and contractility), lipid metabolism, inflammatory pathways, and vessels (via smooth muscle tone and endothelial function). Thyroid hormones have both genomic and nongenomic effects on the cardiac myocyte (modifying expression of calcium regulatory and contractile proteins). Therefore, in an abnormal metabolic state, such a severe hyperthyroidism, derangements can occur in systolic depolarization and diastolic repolarization, in the action potential duration, in the refractory period of the atrial myocardium, and in the atrial/ventricular nodal refractory period. These metabolic effects can produce cardiovascular complications. There is a clear association between dilated cardiomyopathy, diastolic dysfunction, right ventricular dysfunction, and pulmonary hypertension with excess thyroid hormone in thyrotoxicosis.1
Heart failure is the leading cause of mortality in patients with thyroid storm, estimated to be 8 to 25% despite modern advances in its treatment.2,3 Based on clinical findings, the Burch-Wartofsky score assesses the probability of a thyroid storm. A score greater than 45 highly suggests a thyroid storm; our patient scored 85. Due to ongoing cardiomyopathy with signs of heart failure along with atrial flutter based on recent evidence esmolol drip is probably the safest beta-blocker to use in the acute setting due to its very short half-life (9 minutes) avoiding unexpected cardiovascular collapse with longer half-life beta blocker like propranolol (3–4 hours) and allowing quick hemodynamic adjustments at bedside.4 In addition, evidence supports that a single-procedure ablation success rate exceeds 90% for typical and atypical atrial flutter and is associated with decreased hospitalizations, improvement of the LVEF, emergency department visits, development of subsequent atrial flutter, and improved quality of life.5 The early ablation and multidisciplinary approach were the cornerstones in our case.6–8
FOLLOW-UP
Hydrocortisone and methimazole taper with continuous thyroid hormone level monitoring were performed as symptoms and vital signs improved. Goal-directed medical therapy was started for heart failure with a reduced ejection fraction, resulting in the improvement of the clinical course.9
CONCLUSIONS
Heart failure is the leading cause of mortality in patients with thyroid storm, estimated to be 8 to 25% despite modern advancements in its treatment. In patients with high failure along with atrial flutter based on recent evidence esmolol drip is probably the safest beta-blocker to use in the acute setting due to its very short half-life (9 minutes) avoiding unexpected cardiovascular collapse with longer half-life beta blocker like propranolol (3–4 hours). In addition, catheter ablation has a class I indication in patients with heart failure and atrial flutter. Thyroid storm should always be suspected, especially in patients with a new onset of high-output heart failure or tachyarrhythmias.
LEARNING OBJECTIVES
- Multiple cardiovascular complications can occur during uncontrolled hyperthyroidism. The prognosis depends on the complications and associated comorbidities; however, arrhythmias should be considered as a triggered complication and/or perpetuating factor in the heart failure assessment.
- Early consideration of catheter ablation in the setting of atrial flutter and heart failure may improve outcomes.
- Atrial flutter is the second most common in patients with heart failure and hyperthyroidism with a well-known high cure rate after ablation.
- Esmolol is probably the safest beta blocker in thyroid storm with cardiovascular involvement in acute settings or critically ill patients due to its short half-life.
Consent: Informed written consent was obtained from the patient.
REFERENCES
- Razvi S, Jabbar A, Pingitore A, et al. Thyroid hormones and cardiovascular function and diseases. J Am Coll Cardiol 2018;71(16):1781–96. Available from: http://dx.doi.org/10.1016/j.jacc.2018.02.045
- Siu C-W, Yeung C-Y, Lau C-P, et al. Incidence, clinical characteristics and outcome of congestive heart failure as the initial presentation in patients with primary hyperthyroidism. Heart 2007;93(4):483–7. Available from: https://pubmed.ncbi.nlm.nih.gov/17005710/
- Dahl P, Danzi S, Klein I. Thyrotoxic cardiac disease. Curr Heart Fail Rep 2008;5(3):170–6. Available from: https://pubmed.ncbi.nlm.nih.gov/18752767/
- Bokhari SFH, Sattar H, Abid S, et al. Cardiovascular collapse secondary to beta-blocker administration in a setting of coexisting thyroid storm and atrial fibrillation: A case report. Cureus 2022;14(9). Available from: https://pubmed.ncbi.nlm.nih.gov/36277558/
- Boxhammer E, Bellamine M, Szendey I, et al. Impact of cavotricuspid isthmus ablation for typical atrial flutter and heart failure in the elderly—results of a retrospective multi-center study. Front Cardiovasc Med 2023;10. Available from: http://dx.doi.org/10.3389/fcvm.2023.1109404
- Klein I, Danzi S. Thyroid disease and the heart. Circulation 2007;116(15):1725–35. Available from: https://pubmed.ncbi.nlm.nih.gov/17923583/
- Klein I, Ojamaa K. Thyroid hormone and the cardiovascular system. N Engl J Med 2001;344(7):501–9. Available from: https://pubmed.ncbi.nlm.nih.gov/11172193/
- Waqar Z, Avula S, Shah J, et al. Cardiovascular events in patients with thyroid storm. J Endocr Soc 2021;5(6):bvab040. Available from: https://academic.oup.com/jes/article/5/6/bvab040/6168371
- Ross DS, Burch HB, Cooper DS, et al. American Thyroid Association guidelines for diagnosis and management of hyperthyroidism and other causes of thyrotoxicosis. Thyroid 2016;26(10):1343–421. Available from: http://dx.doi.org/10.1089/thy.2016.0229
Article citation: Castillo C, Abdelmalek J, Juarez M. Acute decompensated heart failure in the setting of cavotricuspid isthmus-dependent atrial flutter and thyroid storm. The Southwest Respiratory and Critical Care Chronicles 2024;12(51):14–17
From: Department of Internal Medicine, Texas Tech University Health Sciences Center, Lubbock, Texas
Submitted: 2/27/2024
Accepted: 4/15/2024
Conflicts of interest: none
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.